Depression
Depression hits the invisible illness community hard. While less than 10% of the general population has one or more major depressive episodes per year, one-third of people who live with chronic illnesses deal with depression, and half of those with autoimmune diseases experience depression-like symptoms. In short: if someone has this mood disorder, they. are. not. alone.
How does one know if what they are feeling is clinical depression, and it’s not just a case of the blues? Depression is often diagnosed based on criteria listed in the DSM-5, a diagnostic tool published by the American Psychiatric Association.
Common symptoms of depression include sadness, a flat mood, and a loss of interest in things that used to excite someone. Additional signs of sliding into depression include not eating right, not sleeping well, feeling fatigued, having a hard time concentrating, or having feelings of worthlessness or guilt. Depression sometimes also brings intrusive suicidal thoughts, symptoms that qualify as an emergency—and it’s very important to get help ASAP. Asking a loved one, family member or friend you trust to support you in getting that help can be beneficial.
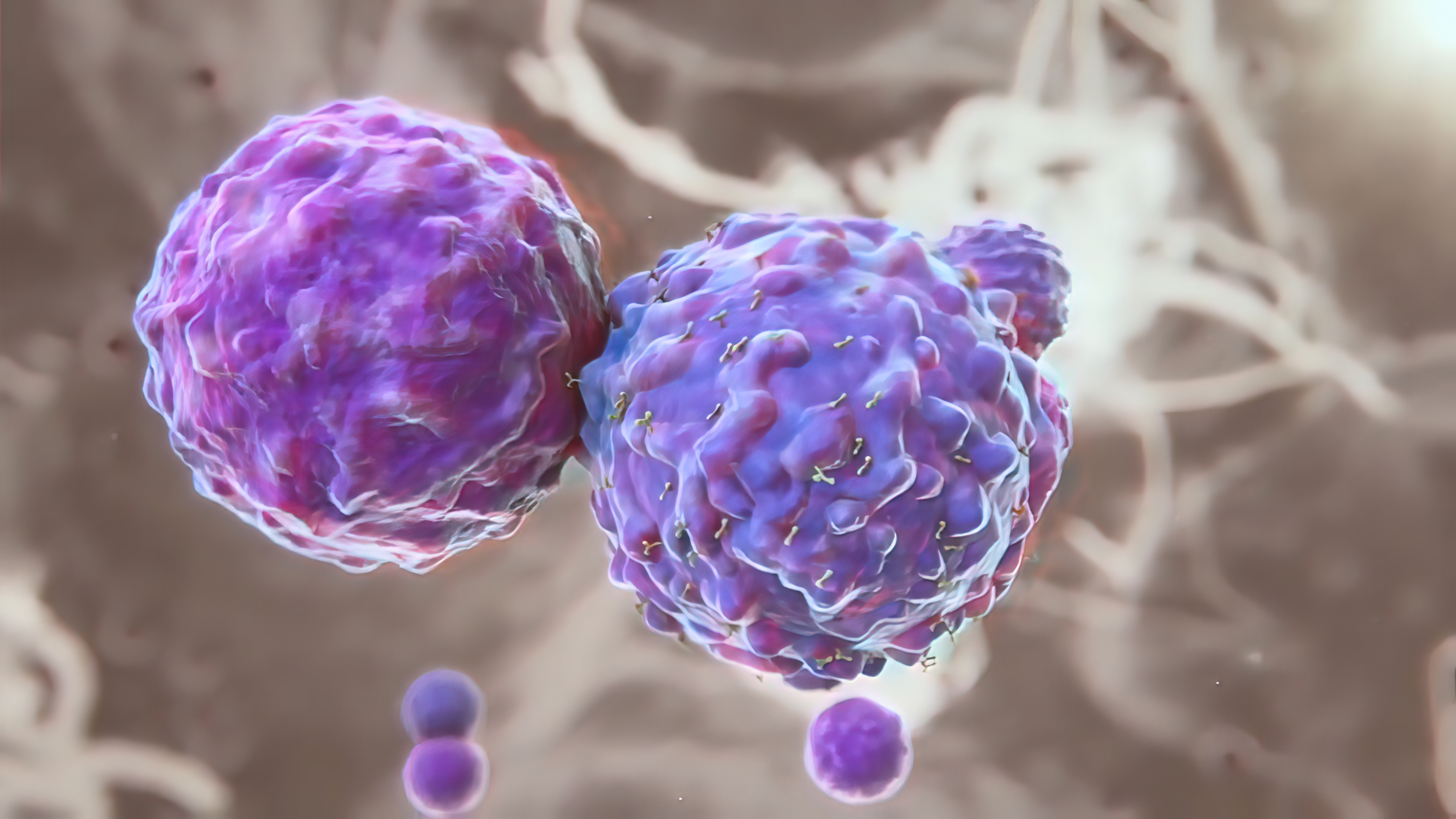
It can be incredibly hard to keep spirits up when someone is dealing with a chronic illness, for all kinds of reasons. In addition to the illness itself and the side effects of treatment, being sick can affect mobility and independence, and can change the way someone lives, their self-perception, and the way others see them. To pile on, their condition can make them feel physically depressed. Inflammation and immune system fluctuations, for example, can affect the brain and lead to behavior abnormalities, including fatigue and depression-like symptoms. Being ill can be a lonely journey—if we let it be. Too many people focus on the primary diagnosis while letting depression go untreated…until they are feeling much worse. But it doesn’t have to be that way.
Depression is treatable. The first step—and it can be a hard one—is asking for help. There’s no one-size-fits-all treatment for this condition, and working with a healthcare provider or mental health professional is recommended, as they can help with understanding symptoms and the possible need for antidepressant medication. In cases of severe depression, hospitalization or inpatient treatment may be recommended to help with mental health. More common treatments include antidepressants, talk therapy, or a combination of both. There are also natural remedies and self-care options to explore, including exercise, relaxation techniques, meditation, yoga, guided imagery, and music therapy. St. John’s wort, an herbal supplement popular for depression, might be effective for some people. There’s also research to support kava, 5-Hydroxytryptophan (5-HTP), and SAM-e supplements, among others.
If you are feeling shame about having depression, or you've been reluctant to get help for any reason, know this: Both of those are common sentiments, but help is out there, and by talking about your experience and seeking treatment, you are helping to break down the stigma that has needlessly hurt others in your shoes.
Resources
- BMJ Open. Complementary therapies for clinical depression: an overview of systematic reviews. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6686993
- National Institute of Mental Health. Major Depression. https://www.nimh.nih.gov/health/statistics/major-depression.shtml
- Natural remedies for depression: Are they effective? https://www.mayoclinic.org/diseases-conditions/depression/expert-answers/natural-remedies-for-depression/faq-20058026
- Mayo Clinic. Depression (major depressive disorder). https://www.mayoclinic.org/diseases-conditions/depression/diagnosis-treatment/drc-20356013
- Cleveland Clinic. Chronic Illness and Depression.
https://my.clevelandclinic.org/health/articles/9288-chronic-illness-and-depression - Canadian Journal of Psychiatry. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4994794